Postbiotics: a step beyond other biotics
The modulation of the gut microbiome has attracted recent interest and we are progressively developing a deeper understanding of the role of microbiota-derived components in human diseases. 1,2
Studies have shown strong evidence that bacterial viability is not essential for imparting health benefits and the term ‘postbiotic’ was created to denote this concept.
ISAPP has recently published a consensus on postbiotics describing them as a “preparation of inanimate microorganisms and/or their components that confers a health benefit on the host”. 3
The ISAPP consensus specifies that viruses (including bacteriophages), vaccines, filtrates without cell components and purified microbial components and metabolites are not classed as postbiotics.
Postbiotics in practice
The positive health impact of postbiotics must be confirmed in the target host which could be either human or animal. The consensus also highlights that, although the gut is not their only site of action, postbiotics must be administered to a host surface such as the oral cavity, gut, skin, urogenital tract or nasopharynx. Injections are outside the scope of postbiotics.
Unless postbiotics have been inactivated under the conditions used to make a product (for example, exposure to atmospheric conditions might inactivate a strict anaerobe), they will require an inactivation step. 3
Several technological strategies are available to inactivate living cells, thereby changing the cell structures of the microbe and/or their physiological function. 4
Thermal processing or heat-treatment (pasteurization, tyndallization, autoclaving) is often used to inactivate microorganisms, and confer enzymatic and microbiological stability on food systems but other technologies (such as drying techniques, electric field, ultrasonication, high pressure, X-rays, ionizing radiation, high-voltage electrical discharge, pulsed light, magnetic field heating, moderate magnetic field and plasma technology) represent useful alternatives. 3
The combined or successive application of less aggressive methods, applied either independently or in tandem with other stresses, such as mild temperature, can also be used to achieve microbial inactivation. 3
The ability of a postbiotic to mediate a health effect may be driven by many different mechanisms, mechanisms acting independently or in combination. These mechanisms may be similar to those of probiotics. 3 However, unlike probiotics, postbiotics are not dependent on the viability of microorganisms and can offer the advantage of a longer shelf-life with maintained efficacy. In general, postbiotics can have both local and systemic effects. 2
- Modulation of the microbiota
Postbiotic compounds can have direct antimicrobial activity (e.g., bacteriocins) and indirectly modulate the microbiota, for example by carrying molecules (e.g., lactic acid) utilized by resident microorganisms to produce substrates with beneficial functions, such as short-chain fatty acids (SCFAs) and butyrate. Furthermore, postbiotics can compete with resident microorganisms for adhesion sites3. - Enhancement of barrier function
Postbiotic components (secreted proteins, EPS or SCFA) can directly enhance epithelial barrier function and/or promote it by reducing inflammation.3 - Modulation of the immune response
In general, local and systemic immune-modulatory activities are exerted by molecular patterns interacting with specific receptors of immune cells. In addition, microbial metabolites can mediate immune effects, influencing a number of immune responses.3 - Modulation of systemic metabolism
Metabolites or enzymes inside and on the surface of the inactivated microorganisms can influence metabolic responses. 3 - Signalling via the nervous system
Microorganisms can produce various neuroactive compounds, vitamins and metabolites that can act on both the enteric and central nervous systems with the potential to modulate behaviour and cognitive function.3

Safety, efficacy & convenience compared to live microorganisms
Safety:
- No known risk of acquisition and retransfer of antibiotic resistance genes
- No known risk of interference with normal colonization of gut microbiota in neonates
- Translocation from gut lumen to blood is unlikely: no known risk of bacteraemia of fungaemia3,5
Efficacy:
- Release of active molecules from the disrupted inactivated cells, passing through the mucus layers and stimulating epithelial cells more directly5
- Absence of viability and cell lysis does not affect postbiotic efficacy and can lead to further and more complex beneficial effects5
- Proven clinical benefits across a wide range of indications3
Convenience:
- Easy to standardize, transport, and store - no need for refrigeration (postbiotics can be stored at room temperature)
- Reliable dosing – not affected by cell viability
- Ready-to-use & good stability - long shelf-life
- Can be administered in conjunction with antibiotic treatment without any loss of efficacy
As Postbiotics do not contain live microorganisms the risks associated with their intake are reduced.
Postbiotics are available as prescription or over-the-counter medications and also as food supplements. Postbiotics are already being used for several therapeutic purposes in humans: for example, Lactobacillus LB and its culture medium are indicated for the treatment of acute, antibiotic-related and chronic diarrhea. Several other indications could benefit from postbiotics showing that they can play a valuable role in clinical practice.
Postbiotic efficacy across a range of indications in adults
| Indication | Postbiotic Strain | Results |
|---|---|---|
| Helicobacter pylori-positive infection (dyspepsia) | Heat-treated Lactobacillus LB plus fermented culture medium | Eradication rates: Triple therapy alone - 72% Triple therapy plus inactivated Lactobacillus LB – 87% (p=.02). |
| Irritable Bowel Syndrome with diarrhea (IBS-D) | Heat-treated Lactobacillus LB plus fermented culture medium | Improved scores for pain, bloating, diarrhea and quality of life. |
| Irritable Bowel Syndrome | Bifidobacterium bifidum | Composite primary endpoint of ≥ 30% improvement in pain and adequate relief of overall IBS symptoms in at least 4 of 8 weeks of treatment. Primary endpoint achieved in 34% active vs. 19% placebo. |
| Chronic diarrhea | Heat-treated Lactobacillus LB plus fermented culture medium | Reduced stool frequency at weeks 2 and 4; overall symptoms improved at 4 weeks in heat-treated Lactobacillus LB group. |
| Obstructive jaundice | Lactobacillus plantarum | Measured intestinal permeability – increased in water in inactivated groups; trend towards normalization in active group. |
| Stress response | Lactobacillus gasseri | In male students sleep quality was improved and diarrhea prevented. Not in females. |
| Chronic stress response | Lactobacillus gasseri | Significant reduction in anxiety and sleep disturbance. Accompanied by EEG changes, reduction in salivary chromogranin and resolution of stress-related microbiota changes. |
| Latent tuberculosis | Mycobacterium manresensis | Increased regulatory T-cell response; well tolerated. |
| Moderate, persistent asthma | Mycobacterium phlei | Symptom scores and spirometry improved. |
| Severe chronic obstructive pulmonary disease (COPD) | Haemophilus influenzae | Reduced severe exacerbations by 63% and exacerbations requiring corticosteroid therapy by 56% and hospitalization by 90%. |
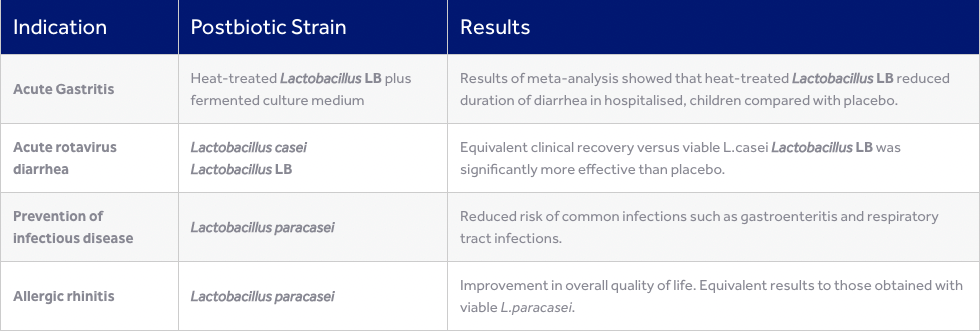
Postbiotic efficacy across a range of indications in children
| Indication | Postbiotic Strain | Results |
|---|---|---|
| Acute diarrhea | Heat-treated Lactobacillus LB plus fermented culture medium | Results of meta-analysis showed that heat-treated Lactobacillus LB reduced duration of diarrhea in hospitalised, children compared with placebo. |
| Acute rotavirus diarrhea |
Lactobacillus casei Lactobacillus LB | Equivalent clinical recovery versus viable L.casei Lactobacillus LB was significantly more effective than placebo. |
| Prevention of infectious disease | Lactobacillus paracasei | Reduced risk of common infections such as gastroenteritis and respiratory tract infections. |
| Allergic rhinitis | Lactobacillus paracasei | Improvement in overall quality of life. Equivalent results to those obtained with viable L.paracasei. |
References:
1 Zolkiewicz et al., Postbiotics—A Step Beyond Pre- and Probiotics. Nutrients (2020). 2 Puccetti et al., Postbiotic-Enabled Targeting of the Host-Microbiota-Pathogen Interface: Hints of Antibiotic Decline? Pharmaceuticals (2020). 3 Salminen, S., Collado, M.C., Endo, A. et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat Rev Gastroenterol Hepatol (2021). https://doi.org/10.1038/s41575-021-00440-6. 4 Belinda Vallejo-Cordoba et al., Postbiotics and paraprobiotics: A review of current evidence and emerging trends. Advances in Food and Nutrition Research (2020). 5 Piqué N. et al. Health Benefits of Heat-Killed (Tyndallized) Probiotics: An Overview. International Journal of Molecular Sciences 2019;20(10).
Experts talk about postbiotics
Discover what our experts say about postbiotics: their definition, benefits over other biotics, and demonstrated health benefits of postbiotics.
What is a postbiotic?
Hear from Professor Colin Hill the reasons why postbiotics are going to be the biotics of the future.
Over the past decade, the term ‘postbiotic’ has appeared quite often in scientific literature in reference to various microorganism-derived preparations used to promote health. This year, the 2021 Consensus issued by the International Scientific Association of Probiotics and Prebiotics (ISAPP) provided a clear definition of a postbiotic.
What are the benefits of postbiotics over living biotics?
In this video, Professor Sarah Lebeer tells us more about the advantages of postbiotics over living biotics and about the five main mechanisms of actions that have been identified for postbiotics.
Postbiotics are inanimate but certainly not inactive. They can modulate, protect and promote multiple functions, while offering several advantages over living microorganisms.
What’s the evidence of human health benefits from postbiotics?
Professor Gabriel Vinderola explains the benefits of postbiotics for both children and adults.
A lot of research has been carried out on postbiotics that includes in vitro, animal and clinical studies. In humans, postbiotics have been shown to reduce the risk of infection and allergic diseases as well as treating gastrointestinal pathologies amongst others.
What is the role of postbiotics in acute diarrhea ?
Dr. Alexis Mosca, gastropediatrician from Robert Debré University Hospital in Paris, answers this question during a symposium presented during the 8th international congress on Probiotics, Prebiotics, Postbiotics in Pediatrics (PPPP).